
Your Guide to ABA Therapy Insurance Coverage for Autism in Texas
For any parent, receiving an autism diagnosis for your child can be an overwhelming experience. Figuring out just what kind of help your child needs, along with who to trust and where to go … that’s all hard enough. Eventually, it hits you — how am I going to pay for the therapy my child needs? Can I get ABA therapy insurance coverage? This guide explains the options — whether you have insurance or not — for accessing Applied Behavior Analysis (ABA) treatment for your child in Texas.
Texas ABA Therapy Insurance Basics
Texas law requires employer insurance plans (plans that are part of employee benefits) to provide “meaningful” autism insurance coverage for children. However, there are some exceptions, especially regarding coverage for ABA therapy. Many, but not all, employer-sponsored plans provide some form of coverage for the following:
- Evaluation and assessment services
- Applied Behavior Analysis (ABA)
- Behavior training and behavior management
- Speech therapy, occupational therapy, and physical therapy
- Medications or nutritional supplements
However, the amount of ABA therapy insurance coverage and patient or beneficiary responsibility (what you owe after insurance pays its part of the bill) varies among employers, insurance companies, and insurance plans. For example, your insurance plan may not cover the same services at the same rates as your neighbor’s plan from the same insurance provider.
Common Insurance Terms To Know
Deciphering what your insurance covers means learning a whole new language. Here’s a list of commonly used insurance terms and definitions. Keep in mind, each insurance plan has its own rules, so confirm with your plan representatives what they cover and what they don’t.
Premium: A monthly cost (sometimes split between pay periods) paid to the insurance company and often partially paid by the employer. Premiums are not applied to out-of-pocket costs.
Patient or beneficiary responsibility: The portion of costs of medical services that the beneficiary pays for before the insurance plan pays its portion.
Co-pay: A set rate you pay for some prescriptions, doctor visits, and other types of services. Not all plans have co-pays, and co-pays do not apply to all services. Co-pays do not typically count toward your deductible.
Co-insurance: A cost-sharing structure in which the insurance company pays a percentage of the care costs and the beneficiary is responsible for the remaining percentage of costs. These costs are usually applied after a deductible is met.
Deductible: A deductible is the amount you pay each year before your health plan begins to share in the cost of covered services. Some medical fees may or may not be included in the deductible.
Out-of-pocket maximum: Out-of-pocket maximum is the most you could pay for covered medical expenses in a year. Most co-pays will count toward your out-of-pocket maximum.
In-network benefits: Most insurance plans have a network of providers that meet the plan’s credential requirements and accept the plan’s reimbursement rates for services. Services from in-network providers are covered at a higher rate for the beneficiary than out-of-network providers.
Out-of-network providers: If a provider does not have a contract with your insurance plan, they’re considered out-of-network. Some plans have some out-of-network benefits, but the amount paid by the beneficiary is usually much higher. If there are no out-of-network benefits, the beneficiary may be responsible for the full price of the service. Providers may also charge additional out-of-network fees.
Preferred Provider Organization (PPO) plans: On a PPO plan, you generally pay less for in-network services, but you usually pay more for premiums. Many PPOs have some out-of-network benefits and a larger network of providers in a larger area. A referral is usually not necessary to see a specialist.
Health Maintenance Organization (HMO) plans: HMOs only cover providers that are in your plan’s network. If a beneficiary uses an out-of-network provider, the beneficiary will have to pay full price for the services, except in emergency situations. HMOs usually have localized networks (only in a certain area), and have lower cost premiums, but higher service costs for beneficiaries. HMOs also generally require a referral by a primary care doctor for any specialist visits.
Quote of Benefits (QOB): A quote of benefits may be available from your medical provider with information from your insurance plan about the rates at which they will pay for covered services and what the beneficiary is responsible for paying. It is always a good idea to double-check these rates directly with your insurance plan.
Pre-authorization: Some plans require pre-authorization before agreeing to cover certain services. Most insurance plans require pre-authorization for ABA therapy services. Insurance companies also often require reauthorization after a certain time period in order to continue covering ABA therapy.
Requirements for ABA Therapy Insurance
Because of the intensity of ABA therapy, most ABA therapy insurance plans require pre-authorization for your child’s initial evaluation and for starting treatment. Most plans also require reauthorization for ongoing services. Each plan has criteria for approving services based on the treatment plan submitted by your child’s Board Certified Behavior Analyst (BCBA).
The pre-authorization process can be overwhelming for any family, but at Thrive Behavior Centers, our goal is to make the process as stress-free as possible. We do most of the work for you — we verify benefits, submit authorization reports, request evaluations and autism therapy insurance coverage, and bill the insurance company on your behalf.
Autism Insurance Coverage Requires a Medical Diagnosis of Autism
Before submitting any requests for ABA therapy insurance, your child will need a medical autism diagnosis. All insurance plans require a medical diagnosis of autism spectrum disorder before authorizing ABA services. The medical diagnosis should also include diagnostic testing for autism and cognitive testing. Plans will require the diagnosis to be conducted by either a medical doctor (M.D.) or a Ph.D.
Professionals who can evaluate for and diagnose autism include the following:
- Developmental pediatricians
- Licensed psychologists
- Some neurologists
- Some pediatricians
A medical diagnosis of autism is different from an educational diagnosis. If your child has been diagnosed with autism through his or her public school district, that diagnosis is not likely to be accepted by your ABA therapy insurance plan. Think of the public education and private medical fields as two different worlds. An educational diagnosis of autism does not cross over to the world of private therapeutic treatment, since it’s based on educational need. In the same way, education professionals may take a medical diagnosis into account, but it does not guarantee special education services in public school districts.
If you have a diagnosis through your child’s school, or you suspect your child may need an evaluation, Thrive Behavior Centers has a list of referrals to providers in the DFW metroplex who evaluate children for autism. Click here to get more information.
How Much Does ABA Therapy Cost Without Insurance?
ABA therapy, especially for younger children with autism, is generally an intensive therapy. The intensity of treatment depends on the child’s needs, but many children need 30–40 hours of intensive ABA therapy to help meet developmental milestones and decrease challenging behaviors.
The costs associated with ABA autism programs are high. Most ABA therapy is one-on-one, meaning each child has a behavior technician — sometimes called a behavior therapist, or Registered Behavior Technician (RBT) — with them at all times to provide direct therapy.
Behavior technicians are not independent practitioners. They must work under the supervision of a Board Certified Behavior Analyst (BCBA). The BCBA is a Master’s-level clinician who manages the child’s case, creates treatment plans, provides parent training, and supervises therapy sessions run by behavior technicians.
The costs associated with hiring and keeping highly qualified treatment teams, as well as the time associated with case management, are high. ABA therapy typically costs about $120 per hour, which can add up to $4,800 per week for a child receiving 40 hours of therapy. That means intensive ABA therapy can cost about $250,000 per year without insurance. Most families aren’t able to afford those costs and need ABA therapy insurance coverage.
Tips for Finding Out if You Have ABA Therapy Insurance
You may feel compelled to call your insurance company immediately after getting a diagnosis. If you follow these tips first, you’ll save yourself time and frustration:
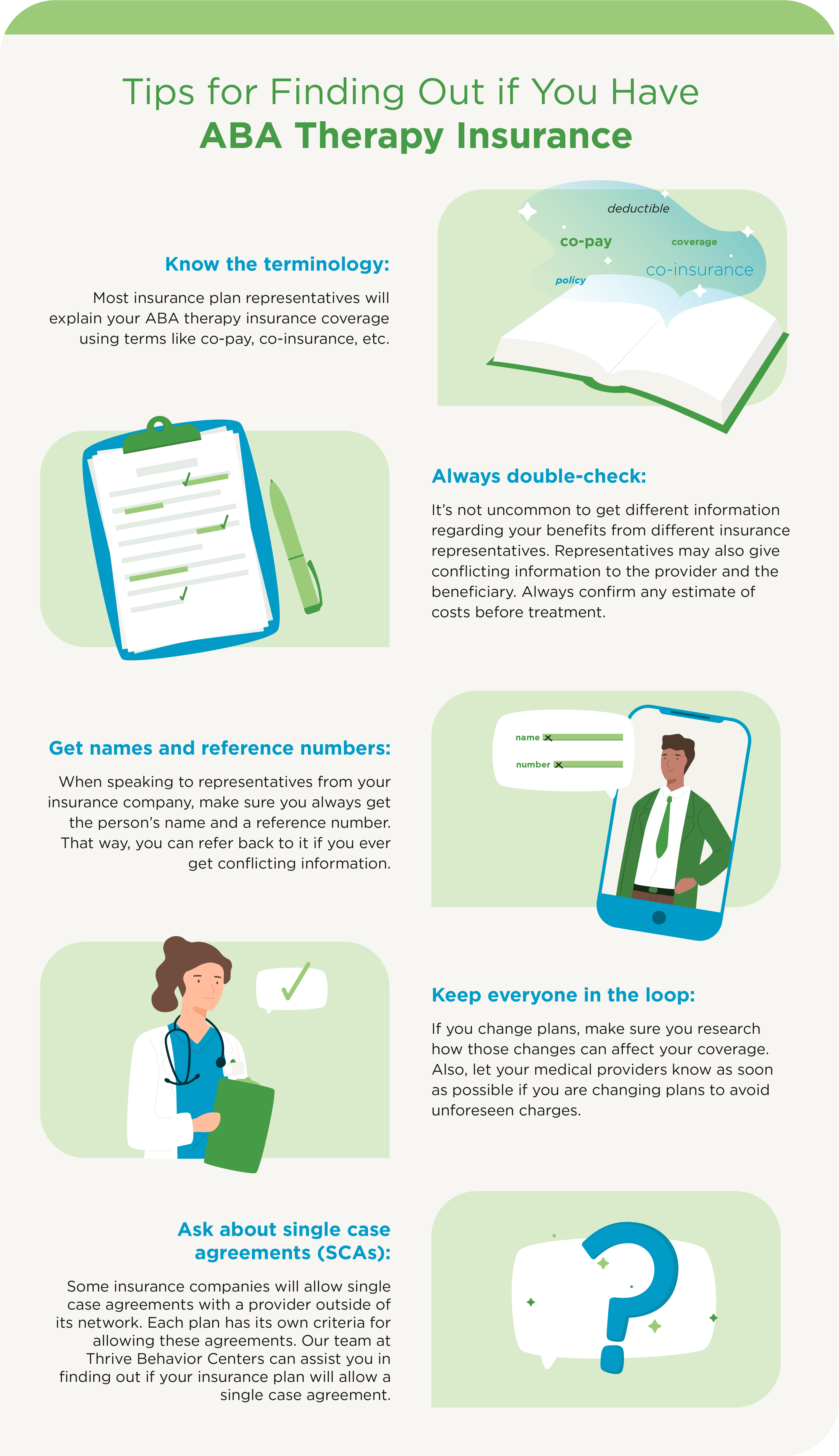
- Know the terminology: Most insurance plan representatives will explain your ABA therapy insurance coverage using terms like co-pay, co-insurance, etc.
- Always double-check: It’s not uncommon to get different information regarding your benefits from different insurance representatives. Representatives may also give conflicting information to the provider and the beneficiary. Always confirm any estimate of costs before treatment.
- Get names and reference numbers: When speaking to representatives from your insurance company, make sure you always get the person’s name and a reference number. That way, you can refer back to it if you ever get conflicting information.
- Keep everyone in the loop: If you change plans, make sure you research how those changes can affect your coverage. Also, let your medical providers know as soon as possible if you are changing plans to avoid unforeseen charges.
- Ask about single case agreements (SCAs): Some insurance companies will allow single case agreements with a provider outside of its network. Each plan has its own criteria for allowing these agreements. Our team at Thrive Behavior Centers can assist you in finding out if your insurance plan will allow a single case agreement.
Thrive Behavior Centers Can Help with ABA Therapy Insurance Questions
Thrive Behavior Centers is an in-network provider for insurance plans including Aetna, Cigna, Tricare, BCBS HMO Magellan, and BCBS PPO Texas. We’re in the process of gaining in-network status with Scott & White, MultiPlan, and Compsych.
But even if we’re not in network, with your insurance plan, you may have options. Some insurance plans will approve a Single Case Agreement, which allows you to use your in-network benefits. We can also direct you to resources that can help cover therapy costs. Helping families get access to ABA therapy is important to us. Contact us with questions.
Texas Law Requirements for ABA Therapy Insurance Coverage
Texas law requires most insurance plans to provide “meaningful” coverage for autism treatment. Bills were passed by Texas lawmakers in 2007 (HB 1919), 2009 (HB 451), and 2013 (SB 1484). Not all insurance plans in the state are included.
These laws are good news for many families with private insurance coverage. However, loopholes allow certain companies to opt-out or reduce coverage for ABA therapy insurance as a child ages.
Coverage Caps
A bill passed in Texas in 2013 eliminated the previous age cap on coverage for autism treatment (it had been 10 years of age). Currently, there is no cap. However, plans can cap coverage for ABA therapy at $36,000 per year for children over 10 years old. Also, to be eligible for coverage, the child must be diagnosed before age 10.
Some insurance plans will also attempt to “titrate,” or reduce, coverage for ABA therapy as a child ages. Insurance plans have their own standards for the authorization of benefits for ABA therapy and don’t always follow clinical recommendations. Often, getting authorization for insurance coverage for intensive ABA therapy can be increasingly challenging as children age, even though there is no formal cap on coverage for plans until age 10.
Exceptions
- State of origin: Find out where, geographically, your health insurance plan originates. Some companies, including those that operate in multiple states, may offer employees an insurance plan that comes from another state. Requirements and laws regarding ABA therapy insurance coverage vary from state to state.
Some states have restrictions on the amount of coverage, age caps, and other regulations that could affect your child’s coverage. Insurance plans are subject to state laws where the plan is issued, not where the beneficiary lives. So even though you live in Texas, Texas laws may not apply to your plan.
Recognizing that a plan is from another state is easy when it’s named something like “XYZ Insurance of North Dakota.” Others may not be as obvious. If your plan is administered out of state, talk to your human resources department or your insurer directly about laws or regulations in that state regarding covered autism treatments. Be sure to ask about limitations or exclusions in ABA therapy insurance coverage.
- Fully funded vs. self-funded: Find out whether your company’s insurance plan is self-funded or fully funded. The Texas mandate only applies to fully funded (large and small) plans, not self-funded plans.
Types of Insurance
There are different types of insurance coverage available to families in Texas — and they each have different levels of coverage.
- Employer-sponsored insurance
- Private employer-sponsored health plans
- Self-funded employer plans
- Fully funded employer plans
- Federal, state, or military employee plans
- Private employer-sponsored health plans
- Medicaid or CHIP (Children’s Health Insurance Program)
- Individual plans
- Purchased through the ACA marketplace (Affordable Care Act, commonly referred to as Obamacare)
- Purchased through an insurance broker
*Click here for more information on various insurance plan types.
Employer Plans for ABA Therapy Insurance
For families who get health insurance through an employer, every year brings new choices. If your child needs ABA therapy, it’s a good idea to examine those choices a little more carefully. In Texas, many employer insurance plans do cover ABA therapy due to the state law requiring insurance coverage of treatment for children with autism. Ask the following questions before assuming your company’s plan covers ABA therapy:
- Do the plans offered by your employer cover ABA therapy?
Texas law requires many employer plans to cover ABA, but there are some exceptions. Self-funded employer plans may not cover ABA therapy for a child with autism. - What are the costs associated with ABA therapy?
Most insurance plans have several ways of splitting covered costs between the insurance company and the beneficiary. Premiums, deductibles, co-pays, co-insurance, and out-of-pocket maximums all play a part in how much money you will actually pay for ABA therapy for your child. Finding this information may be a deep dive into the benefit information provided by your plan during open enrollment. Ask your human resources representative to assist you in finding out more information about ABA therapy. - Are there any coverage caps or limits on the number of visits?
Texas laws only apply to insurance plans that originate in the state of Texas. For plans that originate outside of Texas or self-funded plans, there may be caps or limits on ABA therapy services.
Self-funded vs. Fully Funded ABA Therapy Insurance Plans
In Texas, self-funded plans are a major exception to state laws requiring insurance coverage for ABA therapy with an autism diagnosis. The companies that offer these plans must choose to opt-in to ABA therapy insurance coverage for their employees. Local, state, and national employee groups have lobbied within these companies to convince executives that ABA therapy is the most effective, research-based treatment for children with autism, with many companies choosing to allow ABA therapy coverage for employees and their families. The legal landscape is always changing — so it’s important to understand these differences between self-funded and fully funded insurance plans:
Self-funded plans
In a self-funded health plan, the employer takes on the financial risk of providing health insurance. Larger companies are more likely to have self-funded plans. These plans are not subject to state insurance laws, including the Texas law mandating ABA therapy insurance coverage for children with autism.
Self-funded plans are sometimes called “ERISA” plans — plans governed by the Employee Retirement Income Security Act of 1974, which set minimum standards for self-funded health insurance plans.
It’s not always easy to tell if your company’s plan is self-funded. Some employers contract with insurance companies to administer the plan for them. This means many self-funded plans will operate under the names of common insurance companies, but are not funded by those companies.
Fully funded plans
In a fully funded plan, the company uses another organization to provide its health insurance. This company takes on the financial responsibility for claims and other costs. In Texas, fully funded (large and small) health plans are required to provide ABA therapy insurance coverage for children diagnosed with autism.
Federal, state, and military employer plans
Federal employees covered by the Federal Employees Health Benefit Program (FEHB) are eligible for coverage for ABA therapy for children with autism. This link has more information.
Tricare, the federal government’s military health insurance plan for service members and retirees, also covers ABA therapy. Click here for more information.
Some state healthcare plans in Texas may cover ABA therapy. Whether coverage is available is usually determined by whether the healthcare plan is fully or self-funded. To learn more about fully and self-funded plans, click here.
How To Find Out What Type of Insurance Plan You Have
If your company contracts with a major insurance company, it may look like your plan is fully funded and offers ABA therapy insurance coverage, but that may not be the case. To make sure, you can contact your company’s human resources department and ask whether the plan is fully funded or self-funded.
If the plan is self-funded, ask about coverage for ABA therapy. You should also request information on autism coverage specifically; you may need to contact the plan administrator directly and ask about benefits for ABA therapy for children with autism.
Autism Speaks maintains this list of companies that cover ABA therapy through their self-funded health insurance plans, but it’s always a good idea to double-check with your representative.
Medicaid and ABA Therapy Insurance
Following a hard-fought battle by advocates across the state, Texas Medicaid recipients under age 20 will be able to receive ABA therapy services in February 2022. Beneficiaries must meet the criteria outlined in the Autism Services benefit description and the therapy must be deemed medically necessary. Beneficiaries may contact their Medicaid insurance plan’s benefits representative for additional information as it becomes available.
Options for Families Without Employer ABA Coverage
If your family doesn’t have insurance through your employer, consider these options for adding an individual ABA therapy insurance policy:
- Individual plans purchased through the ACA marketplace
Two different plans are available in North Texas through the ACA (Affordable Care Act, commonly known as Obamacare) marketplace. Depending on income, some families may qualify for tax credits for plans purchased through the ACA marketplace.
Marketplace plans are only available during open enrollment each year (usually from November 15th to December 15th), or if a qualifying event occurs, such as a job loss or loss of insurance coverage from an employer. You can check out plans available on the marketplace by visiting healthcare.gov.
In 2021, the ACA marketplace will be open for an additional enrollment period due to the number of people who may need coverage during the COVID-19 pandemic. The additional open enrollment period is from February 15th to August 15th, 2021. For more information, you can visit healthcare.gov or speak to a health insurance broker.
- Individual plans purchased through a broker
Additional types of individual ABA therapy insurance plans are available for children with autism. These plans may be different from those available on the ACA marketplace and do not qualify for the marketplace plan tax credits. There are some brokers in the DFW area who are very experienced in finding ABA therapy insurance coverage for children with autism.
Tips for Choosing an Individual ABA Therapy Insurance Plan
- Be mindful of open enrollment periods, which are usually from November 15th to December 15th every year, as well as qualifying events (marriage, job loss, etc.). An additional enrollment period is open from February 15th to May 15th, 2021, due to COVID-19.
- Make sure the plan covers ABA therapy. Not all plans that cover autism-related therapies cover ABA.
- Look at total Out-of-Pocket (OOP) costs, not just low premiums, deductibles, or co-pays.
- Double-check co-pay amounts to ensure they apply to ABA therapy (in some cases, co-pay rates may be different).
- Look at both marketplace and individual plans that cover ABA.
- Consider using a broker familiar with ABA therapy coverage. Always ask whether a fee is charged for this service. Some brokers are paid by insurance companies and don’t charge fees for families looking for coverage.
Information provided by Justin Boulet, Vice President of Hipson Benefits. Justin has been helping families find insurance coverage for ABA therapy for more than a decade.
Brokers in the Dallas Fort Worth region with experience helping families find ABA therapy coverage:
- Justin Boulet, Vice President, Hipson Benefits
- Email: jb@hipson.com Phone: 281-493-6862
- Jason Ferrell, Owner, Farrell Financial
- Email: jason@farrell-financial.com Phone: 512-330-1837
Financial Assistance and Grants for Children With Autism
Financial resources are available to help families cover ABA therapy costs and other autism-related treatments and devices. Some are based on income or a child’s age.
The Texas Department of Health and Human Services (HHS) administers one of the autism programs available in the state. The HHS website indicates focused ABA therapy (briefer interventions targeting specific skill areas or challenging behaviors) may be available through a handful of providers in the North Texas region. The therapy is limited to 180 hours per calendar year and other limitations and conditions apply. Click this link for more information.
To learn more about available grants for children with autism, click on the links below:
- Variety of Texas
- National Autism Association – Give a Voice Grant
- National Autism Association Helping Hand Program
- United Healthcare Children’s Foundation
- Resources from The Autism Community in Action (TACA) for help with Communication (AAC) Devices
- 5 Ways to Get a Free Communication (AAC) Device
- Autism Speaks Grant List
- MHMR Tarrant County Resources for Families
- ACT Today
- Anchor of Hope Foundation
- Autism Cares Foundation
- Huckleberry Foundation
- Blooming With Autism
- CJ Torres Family Assistance Grant
- Different Needz Foundation
- Fund it Forward
Ready to get our team’s support to start the insurance preauthorization process? Get started today.
Related Articles
Parent Resource
August 17, 2023
Even with insurance coverage, medical and therapy bills for a child with autism can stretch any family's budget. There are[...]
Parent Resource
August 17, 2023
At Thrive Behavior Centers, our team is committed to providing safe, ethical and effective ABA therapy for your child.
Parent Resource
November 22, 2021
What To Do if You're Concerned About an Autism Diagnosis It may be a friend, a teacher, a day-care provider,[...]




